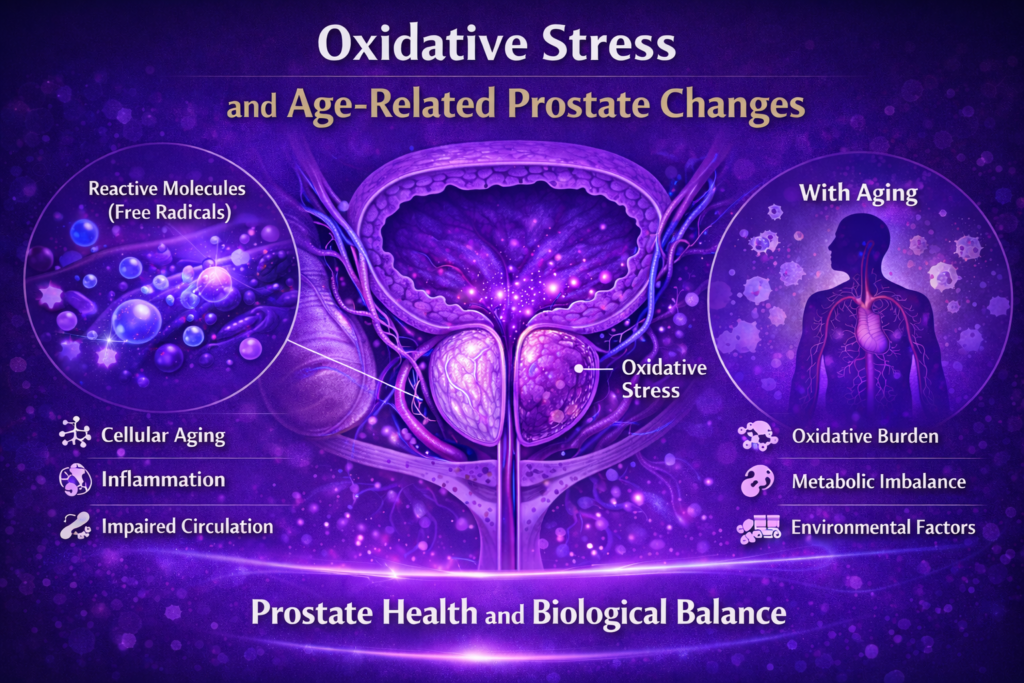
As men age, various biological processes gradually influence how tissues function and adapt. One of the most widely studied processes in age-related health research is oxidative stress. In recent years, researchers have increasingly explored how oxidative stress may relate to prostate changes observed later in life.
Understanding oxidative stress provides valuable context for how inflammation, circulation, and cellular aging intersect in prostate health.
What Is Oxidative Stress?
Oxidative stress refers to an imbalance between reactive molecules—often called free radicals—and the body’s ability to regulate them through protective mechanisms. These reactive molecules are natural byproducts of normal metabolism and cellular activity.
Under balanced conditions, the body maintains systems that manage oxidative activity. Over time, however, these regulatory systems may become less efficient.
Why Oxidative Stress Increases With Age
Age-related changes in metabolism, circulation, and cellular repair can influence how effectively the body controls oxidative processes. Factors commonly associated with increased oxidative stress include:
- reduced mitochondrial efficiency
- changes in antioxidant systems
- cumulative environmental exposure
- metabolic imbalance
These factors help explain why oxidative stress is frequently studied in relation to aging tissues, including the prostate.
🎥 Video Overview: Oxidative Stress and Prostate Health
(A brief visual explanation exploring how oxidative processes are studied in relation to prostate aging.)
Oxidative Stress and Prostate Tissue
Prostate cells, like all cells, rely on balanced oxidative signaling for normal function. Research explores how prolonged oxidative stress may influence cellular structure, signaling pathways, and tissue responsiveness over time.
Rather than acting alone, oxidative stress interacts with inflammatory and vascular processes, shaping the local environment within prostate tissue.
Interaction With Inflammation and Circulation
Oxidative stress, inflammation, and circulation are closely interconnected. Changes in blood flow may affect oxygen delivery and waste removal, while inflammatory activity can increase oxidative signaling.
Researchers examine how these processes reinforce one another, particularly in age-related contexts where regulatory balance becomes more difficult to maintain.
Cellular Adaptation and Long-Term Balance
Cells possess adaptive mechanisms designed to respond to oxidative challenges. Over time, however, persistent stress may influence how effectively cells maintain structural and functional integrity.
From a research perspective, age-related prostate changes are often viewed as the result of long-term biological adaptation, rather than isolated events.
Lifestyle Factors and Oxidative Balance
A growing body of research examines how lifestyle patterns influence oxidative balance across the body. Factors commonly studied include:
- physical activity
- nutritional patterns
- metabolic health
- sleep quality
- exposure to environmental stressors
These factors are evaluated for their systemic effects rather than prostate-specific actions alone.
Interpreting Oxidative Stress Research Responsibly
🎥 Video Overview: Oxidative Stress and Prostate Health
(A brief visual explanation exploring how oxidative processes are studied in relation to prostate aging.)
It is important to approach oxidative stress research with nuance. While associations are well documented, individual responses vary, and oxidative processes serve both signaling and protective roles in the body.
Research emphasizes balance rather than elimination of oxidative activity, highlighting the complexity of biological regulation.
Final Thoughts
Oxidative stress represents a central process in aging research and provides important context for understanding age-related prostate changes. Rather than acting independently, oxidative stress interacts with inflammation, circulation, and cellular adaptation over time.
Viewing prostate health through this lens supports a more integrated understanding—one that emphasizes long-term balance and systemic health rather than isolated factors.