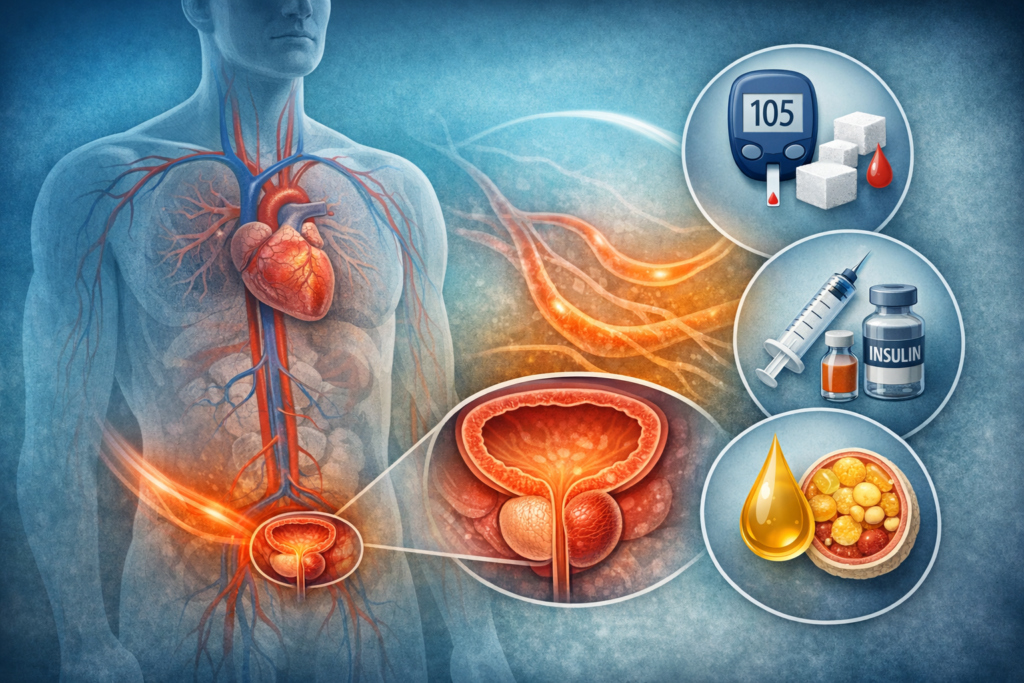
Prostate health does not exist in isolation. Like many tissues in the body, the prostate responds to broader physiological signals influenced by metabolism, circulation, and hormonal regulation. In recent years, researchers have increasingly explored how metabolic health may shape the environment in which age-related prostate changes occur.
Understanding this connection requires looking beyond the prostate itself and examining systemic patterns that influence tissue function over time.
What Is Metabolic Health?
Metabolic health generally refers to how efficiently the body regulates energy, blood sugar, lipid balance, and inflammatory signaling. It reflects the coordination of multiple systems, including:
- glucose regulation
- insulin signaling
- lipid metabolism
- body composition
- vascular responsiveness
Rather than a single measurement, metabolic health represents a pattern of internal balance that affects nearly every organ system.
🎥 Video Overview Video Overview: Metabolic Health and Prostate Function
(A brief visual explanation exploring how systemic metabolic patterns relate to long-term prostate health.)
The Prostate Within a Metabolic Context
Prostate tissue depends on adequate blood flow, oxygen delivery, and balanced cellular signaling. These processes are closely connected to metabolic function.
When metabolic regulation shifts over time, it may influence:
- inflammatory activity
- vascular tone
- hormonal signaling
- cellular stress responses
Researchers examine these interactions as part of a broader effort to understand how systemic physiology shapes age-related tissue adaptation.
Metabolism and Inflammatory Signaling
Low-grade inflammatory activity is often discussed in aging research. Metabolic patterns can influence how the body regulates inflammatory pathways, particularly over long periods.
Rather than acting independently, metabolic regulation and inflammatory signaling are interconnected. Shifts in metabolic balance may alter how tissues respond to normal age-related changes, including those observed in the prostate.
Insulin Sensitivity and Cellular Regulation
Insulin is widely recognized for its role in glucose regulation, but it also functions as a signaling molecule that influences cellular growth and communication.
Research explores how long-term changes in insulin sensitivity may interact with hormonal pathways and tissue responsiveness. While these mechanisms are complex, they highlight the importance of viewing prostate health within a broader systemic framework.
Body Composition and Hormonal Environment
Body composition influences metabolic regulation and endocrine balance. Adipose tissue, for example, is metabolically active and contributes to signaling pathways that extend beyond energy storage.
Age-related shifts in body composition may shape hormonal and inflammatory contexts that indirectly affect prostate tissue adaptation over time.
Vascular Function and Metabolic Regulation
Metabolic health and vascular function are closely linked. Efficient blood flow supports oxygen delivery and cellular waste removal, processes that are essential for maintaining tissue equilibrium.
Because the prostate relies on microvascular circulation, researchers often examine how systemic metabolic patterns may influence local vascular conditions.
🎥 Video Overview Video Overview: Metabolic Health and Prostate Function
(A brief visual explanation exploring how systemic metabolic patterns relate to long-term prostate health.)
Interpreting Research Responsibly
It is important to emphasize that associations observed in metabolic research do not imply direct causation. Prostate health reflects the interaction of multiple biological systems rather than a single metabolic variable.
Current evidence supports a systems-based perspective: metabolic regulation, vascular function, inflammatory balance, and hormonal signaling operate together in shaping long-term physiological outcomes.
Final Thoughts
Metabolic health represents a foundational element of systemic physiology. Rather than acting as an isolated factor, it influences the broader biological environment in which age-related prostate changes occur.
Viewing prostate function through a metabolic lens encourages a more integrated understanding—one that connects local tissue adaptation to whole-body regulation over time.