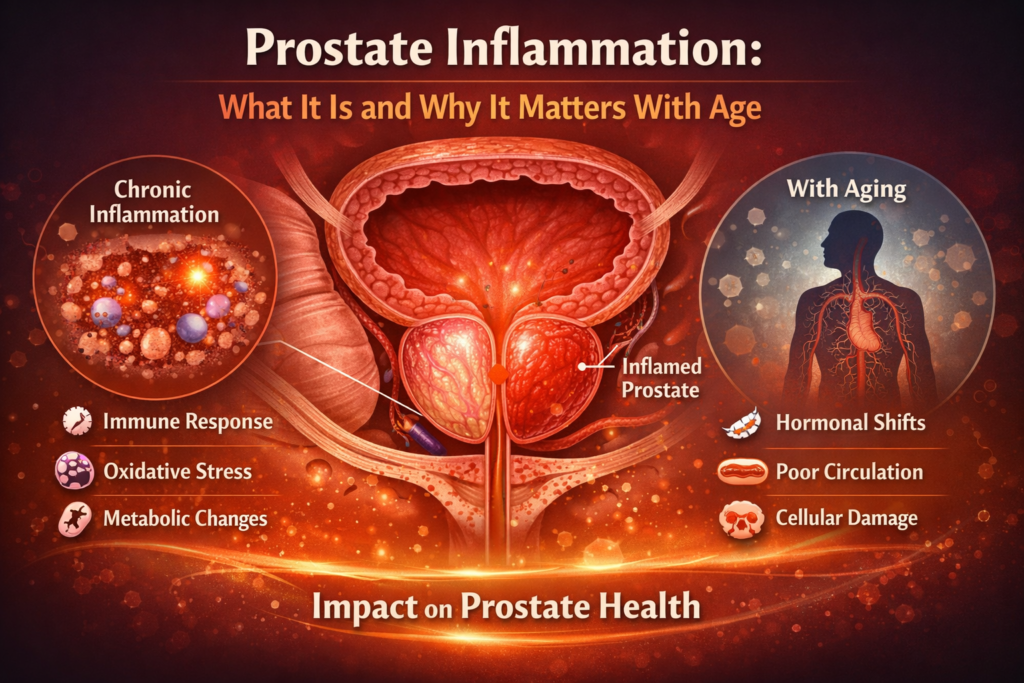
As men age, changes in the prostate are common and often discussed in terms of size or urinary symptoms. Less frequently explained, however, is the role of inflammation in prostate health. Research increasingly suggests that inflammatory processes may influence how prostate changes develop over time and how symptoms are experienced.
Understanding prostate inflammation helps clarify why prostate health is closely connected to broader metabolic and immune-related processes, particularly later in life.
What Is Prostate Inflammation?
Inflammation is a natural biological response designed to protect tissues from injury or infection. In the prostate, inflammatory activity can occur for various reasons, including immune responses, tissue stress, or age-related changes.
Importantly, inflammation does not always indicate infection or disease. In many cases, it reflects low-grade, chronic processes that develop gradually and may not produce obvious symptoms at first.
Acute vs. Chronic Inflammatory Processes
From a research perspective, prostate inflammation is often discussed in two broad contexts:
- Acute inflammation, which tends to be sudden and more noticeable
- Chronic, low-grade inflammation, which may persist over long periods with subtle effects
Age-related prostate changes are more commonly associated with chronic inflammatory patterns rather than acute events.
Why Inflammation Becomes More Relevant With Age
As the body ages, regulatory systems involved in immune response and tissue repair can become less efficient. This may lead to prolonged inflammatory signaling in various tissues, including the prostate.
Factors commonly associated with increased inflammatory activity include:
- metabolic imbalance
- oxidative stress
- reduced circulation efficiency
- changes in immune regulation
These factors help explain why inflammation is frequently studied alongside prostate enlargement and functional changes.
Inflammation and Prostate-Related Symptoms
Research explores how inflammatory activity may influence prostate-related symptoms by affecting tissue structure and signaling pathways. While inflammation is not the sole cause of symptoms, it may contribute to increased sensitivity, tissue stiffness, or altered local responses.
Not all men with prostate inflammation experience noticeable symptoms, which highlights the complexity of how inflammation interacts with individual physiology.
Lifestyle Factors and Inflammatory Balance
A growing body of research suggests that overall lifestyle patterns can influence inflammatory balance throughout the body. While no single factor determines outcomes, certain habits are consistently associated with inflammatory regulation.
These include:
- regular physical activity
- balanced nutrition
- metabolic health
- stress regulation
- sleep quality
From a research standpoint, these factors are studied for their role in systemic inflammation rather than prostate-specific effects alone.
Interpreting Inflammation Research Responsibly
🎥 Video Overview: Inflammation and Prostate Health
(A short visual explanation exploring how inflammatory processes are studied in relation to prostate aging.)
It is important to interpret inflammation-related research with caution. Associations observed in studies do not always imply direct causation, and individual responses vary widely.
Inflammation is one component of a broader physiological picture, interacting with hormonal, vascular, and metabolic systems rather than acting independently.
Final Thoughts
Prostate inflammation is a topic of growing scientific interest, particularly in the context of aging. Rather than representing a single condition, inflammatory processes reflect complex biological interactions that may influence how prostate changes develop over time.
Viewing prostate health through the lens of inflammation supports a more integrated understanding—one that emphasizes overall health, balance, and long-term physiological context rather than isolated symptoms.